Jaw Inflammation
Jaw inflammations can manifest in various forms and pose a health burden for the patient. Almost all forms of jaw inflammation involve a deterioration of the jawbone, visible on X-rays as a dark area (known as radiolucency).
Inflammations in the jawbone can be acute and very painful, or they can be chronic and show no associated pain. This characteristic makes this medical condition particularly insidious, as individuals may be affected for years without being aware of the jaw inflammation.
What is Jaw Inflammation?
Jaw inflammation refers to any form of inflammation in the jawbone or the surrounding soft tissues. If only the jawbone is affected, the condition is also referred to as jawbone inflammation. Such a jawbone inflammation is also known as jaw osteitis, derived from “Os” (Latin for bone) and “Itis” (Latin for inflammation). Jaw inflammations have diverse causes and can present in different ways, being either acute and painful or chronic and virtually painless. The most significant issue with jaw inflammations is the impact on health, with chronic and persistent inflammations potentially weakening the body. Therefore, it is crucial for jaw inflammations to be diagnosed and professionally treated.
Causes of Jaw Inflammation
Jaw inflammations can develop in various ways, with different bacteria in the oral cavity playing a central role. If pathogenic (disease-causing) bacteria penetrate the jawbone, they can cause inflammation of varying types. The nature of the inflammation depends significantly on the bacterial composition, the route of entry, and the immune system’s response.
Tooth Decay (Caries) and its Consequences
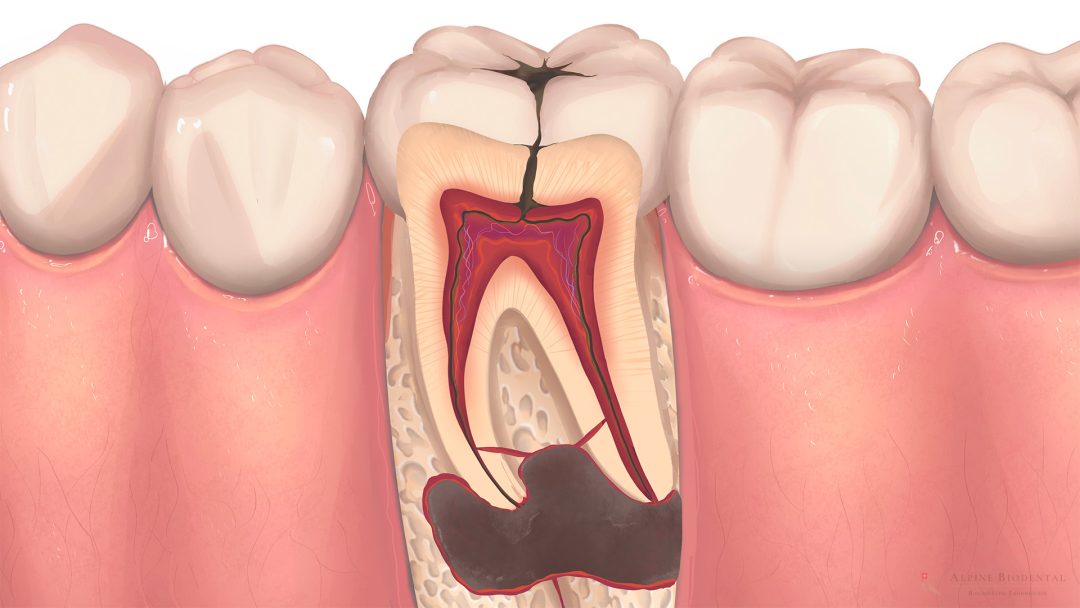
Caries bacteria convert sugar from food into acid. This acid is capable of “etching” decay into the tooth structure, recognizable as a dark spot and hole in the tooth. If the decay penetrates the depth of the tooth, destroying enamel and dentin, the tooth nerve is damaged. Bacteria enter the nerve, causing the tooth to die—referred to by dentists as a devitalized tooth. The infiltrated bacteria travel through the tooth nerve into the jawbone, leading to inflammation at the root tip, known as tooth root inflammation.
Periodontitis and Peri-Implantitis
Periodontitis bacteria are also dangerous and can establish themselves between the gum and tooth, causing gum inflammation (gingivitis) and later, periodontitis. Periodontitis not only results in the loss of the tooth-supporting structure but also leads to inflammation of the jawbone around the tooth. In cases of chronic and prolonged periodontitis, the bone can be so extensively damaged that teeth may lose their support. These bacteria can cause peri-implantitis around a dental implant, where the jaw inflammation spreads around the implant.
Wisdom Teeth
Wisdom teeth typically erupt between the ages of 17 and 25 as the final set of teeth in dental development. Often, wisdom teeth have insufficient space in the jaw, causing them to erupt at an angle and create areas for debris accumulation. Bacteria can nest in these debris-prone areas, leading to jaw inflammation, which can be painful.
The eruption of wisdom teeth may result in Dentitio Difficilis due to space constraints. This refers to a challenging tooth eruption, where the partially erupted wisdom tooth can become severely inflamed. Read more about this in the Wisdom Tooth Surgery article.
Tooth Extraction
Tooth extraction involves the removal of a tooth. After a tooth is extracted, harmful bacteria can infect the open wound, leading to a painful postoperative bone inflammation. During tooth extraction, it is crucial to operate with care and adhere to various protective measures to avoid jaw inflammations.
If the bone defect following a tooth extraction heals with fatty tissue and does not mineralize, it can lead to the development of a chronic FDOJ/NICO jaw inflammation.
Root Canal treated Teeth
Teeth that have undergone root canal treatment are not supplied with blood, nerves and lymph, which means that important functions cannot be carried out. Root-treated teeth have no functional immune system and are more susceptible to bacterial colonization. As a result of bacterial spread, dead teeth often exhibit tooth root inflammations more frequently than healthy, vital teeth.
Foreign Bodies in the Jawbone
Due to previous dental treatments, foreign bodies can penetrate the jawbone, causing bone inflammation. Examples of such foreign bodies include amalgam fragments, overpressed root filling material, or broken tooth fragments. To stop the prolonged stress, these foreign bodies should be carefully removed from the jawbone.
The majority of jaw inflammations have a bacterial origin. Therefore, optimizing oral flora is a crucial prerequisite for preventing future inflammations in the jaw. Please read more about building oral flora.
Symptoms of Jaw Inflammation
To better explain the symptoms, jaw inflammations are divided into acute and chronic categories. For easy understanding, remember: Acute inflammations are painful, while chronic inflammations are more inconspicuous and develop slowly.
Acute Inflammation
Acute forms of jaw inflammation are usually accompanied by intense pain, causing sleepless nights for the patient. The affected area feels swollen, warm, and red. Swelling, warmth, and redness are typical symptoms of acute inflammation. Patients complain of pronounced, throbbing, and radiating pain—every movement and touch is painful.
Occasionally, an abscess may form (bacteria migrate into the soft tissues of the cheek or tongue), leading to the accumulation of pus, and pus discharge may be noticeable.
The acute, painful inflammation often originates from a tooth with deep decay – the tooth is sensitive to pressure and touch. However, periodontitis, a wisdom tooth, or a previous tooth extraction can also lead to acute inflammation with severe pain.
To prevent the spread of inflammation, acute jaw inflammations should be treated as quickly as possible. A swollen eye, as well as sore throat and difficulty swallowing, are signals that a dangerous spread has begun. Since this condition can be potentially life-threatening, prompt medical attention should be sought.
Chronic Inflammation - Silent Inflammation
Chronic jaw inflammations are more common than acute ones, often inconspicuous, and painless. Due to their subtle symptoms, they are also referred to as silent inflammation. They can remain unnoticed in the jaw for years, making them potentially hazardous to health. The bacteria present in chronic jaw inflammations can spread throughout the entire body (focus of inflammation), keeping the immune system in a constantly active state. This continuous activation places a strain on the individual’s energy reserves, leading to fatigue and exhaustion. The body’s general tendency for inflammation is heightened, potentially causing additional generalized symptoms. Due to the proximity to the brain and the good blood supply to the head, the negative impact of jaw inflammations on the body can be pronounced.
Types of Jaw Inflammations
Depending on the cause, location, and immune response, there are different types of jaw inflammations that can occur acutely and/or chronically. The following categorization provides a good overview of the various forms of jaw inflammations. To maintain brevity, not all forms will be discussed.
Abscess
An abscess is always acute and is accompanied by intense pain and swelling. The cheek becomes swollen, and a throbbing pain spreads. An encapsulation with pus forms in the abscess, which must be opened and drained by a dentist or oral surgeon. It is crucial to treat the cause of the inflammation.
Jaw Cyst
The jaw cyst is a cavity in the bone filled with fluid and lined externally by epithelium. Jaw cysts can develop, for example, at the root tip of diseased teeth or around wisdom teeth. As jaw cysts expand over time and increase in volume, they can become quite large and destroy a significant amount of bone tissue. The course of a jaw cyst is typically chronic and painless, but infection of a cyst is possible, leading to the emergence of pain. The therapy involves the complete removal of the jaw cyst and addressing the cause of the cyst.
Dentitio Difficilis
Dentitio Difficilis describes inflammation during tooth eruption and is also known as “difficult tooth eruption.” Dentitio Difficilis is particularly common with partially erupted (partially retained) wisdom teeth. This type of inflammation is more acute and causes severe pain. The tooth should be minimally invasively removed in a wisdom tooth extraction.
Inflammation after Wisdom Tooth Extraction/Tooth Removal
Bone inflammation can occur after both wisdom tooth surgery and general tooth removal. After the tooth is removed, an open wound remains, which can become infected. Bacteria from the oral cavity enter and cause inflammation of the jawbone. The course is acute and painful. A very painful form is called Alveolitis Sicca, a dry and unprotected wound that has been fully bacterially contaminated. Please avoid frequent rinsing of the mouth and the area where the tooth was located after tooth removal. Natural bleeding into the empty socket is essential for healthy, inflammation-free healing.
At Alpine BioDental, wisdom tooth extraction or tooth extraction is accompanied by various precautions to avoid complications. In most cases, the use of antibiotics can be avoided.
FDOJ/NICO
FDOJ (fatty-degenerative osteolysis in the jawbone) or NICO (neuralgia-inducing cavitational osteonecrosis) are chronic inflammations characterized by the deposition of fat in the jawbone. In FDOJ/NICO, large amounts of Rantes can be produced, leading to a permanent burden on the entire body. The term NICO is misleading because neuralgia rarely occurs.
FDOJ/NICO is most reliably diagnosed using CaviTAU® ultrasound diagnostics, a special bone density measurement of the jawbone, supplemented by CBCT X-ray diagnostics.
Diagnosis of Jaw Inflammation
There are two reliable and proven methods for diagnosing jaw inflammations. These methods are based on X-rays or ultrasound and are applied in our practices for secure diagnostics.
Diagnosing Jaw Inflammations in X-rays
Jaw inflammation can be well depicted in X-rays, with 3D X-rays, known as cone beam computed tomography (CBCT), being particularly ideal. Through CBCT examination, precise three-dimensional representations of the jawbone can be created. The dentist can inspect each layer precisely, clearly differentiating inflammatory bone changes from healthy bone. Inflammations are recognizable as dark, poorly mineralized areas.
CaviTAU® Bone Density Measurement with Ultrasound
CaviTAU® ultrasound diagnostics can reproducibly display bone density. Non-mineralized areas in the jaw provide an indication of inflammation. These inflamed areas in the jawbone can be clearly distinguished from mineralized, healthy bone. This technique was specifically developed for the visualization of fatty-degenerative inflammations of the jaw (FDOJ/NICO) and should be performed before surgery.
Treatment of Jaw Inflammations
All jaw inflammations are generally treated in a similar manner. The primary step is to eliminate the cause of inflammation, which involves addressing problematic bacteria and the source of contamination (e.g., diseased tooth). Subsequently, complete surgical removal of the jaw inflammation itself is performed.
Jaw Inflammation and Antibiotics/Bacteria
As explained in the section “Causes of Jaw Inflammation,” pathogenic bacteria have a significant influence on the development of inflammations in the jaw. These bacteria should be eliminated for the complete treatment of jaw inflammation. Many dentists prescribe antibiotics, such as Amoxicillin or Clindamycin, to eliminate bacteria. At Alpine BioDental, we strive to avoid the use of antibiotics and instead utilize antibacterial alternatives (e.g., ozone). In rare cases, antibiotic administration may still be necessary.
Removal of the Causative Contaminated Area
The bacterial invasion of the bone and the development of bone inflammation typically result from a contaminated area or connection in the bone. This includes:
- Damaged teeth
- Partially erupted wisdom teeth
- Deep gum pockets
- Bone defects around old implants
- Unfavorable tooth contacts where food residues get stuck
Such areas will repeatedly lead to inflammations and should be eliminated as part of the treatment. If tooth extraction is necessary, compatible ceramic implants can be immediately placed, following the concept of immediate implantation. This approach can often avoid the need for later bone augmentation.
Jaw Inflammation and Surgery
The manifested inflammation in the bone requires thorough cleaning and removal. During surgery, the contaminated area through which bacteria entered (e.g., a damaged tooth, partially retained wisdom tooth) is also removed. The operation includes disinfecting the wound (e.g., with ozone) and using a personalized wound dressing (e.g., with A-PRF). At the end of the operation, the wound edges are correctly adapted with sutures, protecting the wound and enabling rapid healing (known as primary wound healing).
Home Remedies for Jaw Inflammation
Many people wonder what helps with jaw inflammations and which home remedies they can use. There are some home remedies that can provide temporary relief. However, since the root cause of the problem is the contaminated area that allows bacteria to enter the bone, true healing will only occur once this is completely eliminated.
Home remedies that may provide relief include:
- Baking soda: Dissolve baking soda in a glass of warm water and rinse several times a day. Baking soda can buffer bacterial acids and alleviate inflammation.
- Black seed oil: Black seed oil can contain inflammation and acts as a natural pain reliever. Take 1-2 tablespoons throughout the day.
- Clove: Chew on the stem of a clove. The substances released can alleviate pain.
Prevention of Jaw Inflammations
If you develop jaw inflammation, correct prophylaxis (prevention) is important. Two points are essential for prophylaxis and should be followed.
- Build up oral flora: By various measures, pathogenic bacteria should be eliminated, and healthy ones strengthened. This is ideally achieved through the regular application of ozone and plasma, as part of full mouth disinfection, and tooth cleaning.
- Preventing the formation of contaminated areas: Efforts should be made to avoid the formation of contaminated areas through which bacteria can enter the bone in the future. This requires timely detection and correction of cavities, periodontitis, leaking fillings, etc. It necessitates regular check-ups with the dentist. New ceramic fillings and ceramic crowns should have correct anatomy to prevent food debris from getting stuck between the teeth.
Dr. med. dent. Josephine Phillips
Jaw inflammation should be removed atraumatically and thoroughly at the same time. Our experts will be happy to answer any questions you may have.

Frequently asked Questions about Jaw Inflammations
Jaw inflammation can have a serious impact on health. Correct diagnosis and treatment by a dentist is important in order to restore a stable situation. Here you will find the answers to frequently asked questions.
The cause of jaw inflammation should be treated by a surgically experienced dentist. Schedule an appointment with a specialized dentist or a specialist in oral surgery.
If the pain persists more than 5 days after tooth extraction, a jaw inflammation may have developed. You should schedule an appointment with your dentist. To limit bone loss, it is advisable to promptly insert a dental implant, which serves as a replacement tooth and stabilizes the existing jawbone.
For jaw inflammation, you should contact an experienced dentist or a specialist in oral surgery (oral surgeon). In the case of extensive inflammations, going to a hospital is the right choice.
Bone inflammation always poses a health risk. Acute jaw inflammations can lead to a dangerous spread towards the eye or throat. Chronic inflammations (silent inflammation) result in a permanent, unnoticed burden on the body.
Swelling behind the last molar can occasionally develop, often related to a lack of space. Precise diagnosis by a dentist can help identify the cause of the swelling.
To answer this question, the cause of tooth pain should first be determined. Occasionally, tooth pain can go away on its own. However, if a jaw inflammation has developed, dental treatment is essential.
Further information
The information listed contains relevant topics for a better understanding.
