Gingivitis
Tenderness, sensitivity or bleeding of the gums can be a sign of “gingivitis”. Gingivitis is an inflammatory reaction at the gum line which is caused, among other things, by bacterial biofilms. Therefore, gingivitis is commonly referred to as “gum inflammation”. We offer in-depth knowledge and a biological approach to the development, diagnosis and treatment options of this widespread disease. Advanced gingivitis can progress to periodontitis – the inflammation of the periodontium, which is the area between the teeth and the jawbone.
Gingivitis symptoms
When gingivitis is suspected, it is important to recognize the signs and act quickly. Here are some symptoms that may indicate this common oral health problem:
- Redness and swelling: These are the first signs of gingivitis. Your gums will be red, swollen and possibly sensitive when this happens
- Bleeding gums: If your gums bleed when you brush or floss, this could be a clear sign of gingivitis
- Pain: The pain is usually mild, but can be severe and affect the whole jaw.
- Gum inflammation with pus: In advanced gingivitis, pus may form between the tooth and the gum, which is an indication of chronic infection. This requires urgent dental treatment.
- Swollen cheek: In severe cases of gingivitis, there may be visible swelling on the face.
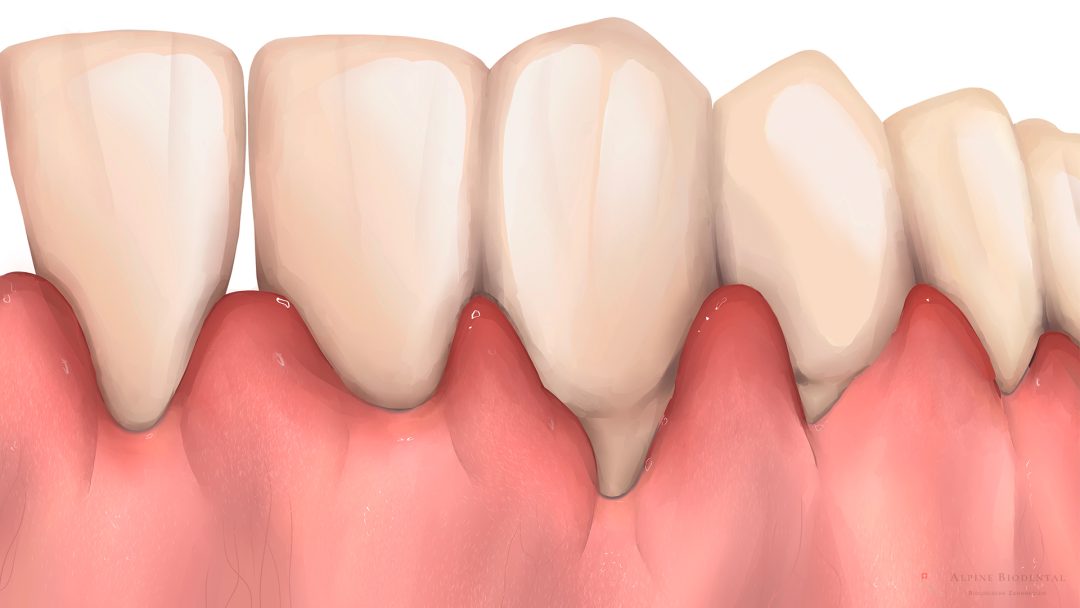
- Receding gums: If you notice that your teeth look "longer", this could indicate gum recession, a symptom of advanced gingivitis.
Please note that these symptoms can also indicate other health problems. Therefore, it is important to consult a dentist if you suspect that you have gingivitis.
Gingivitis treatment
Gingivitis is easily treatable with the right strategies. There are effective remedies that help very well. We offer valuable information below on what to do about gingivitis.
Remedies for gingivitis
In cases where gingivitis is caused by a bacterial infection, an antibiotic remedy for gingivitis is recommended. These remedies contain antibiotics that help eliminate the bacteria causing the inflammation.
In biological dentistry, we try to avoid antibiotics as much as possible. Here, it is recommended to seek out the essential oils appropriate for the predominant bacterial spectrum that will promote their healthy oral microbiome individually. This can be determined by an “Aromatogram”.
Medications for gingivitis
There are several medications used for gingivitis. These primarily include antibiotics and pain relievers, such as ibuprofen.
At Alpine BioDental, we try to treat gingivitis without the use of medications. With the use of ozone, we can optimize the bacterial flora. Natural painkillers also help to avoid the use of chemical painkillers.
Home remedies for inflammation in the mouth
There are proven home remedies that can reduce inflammation in the mouth.
- Salt water rinses: Salt water acts as a natural disinfectant. Stir a teaspoon of salt into a glass of warm water and rinse your mouth with it several times a day. You can also add some baking soda.
- Chamomile tea: Chamomile is known for its anti-inflammatory properties. Rinse your mouth with chamomile tea or soak a cotton ball with the tea and place it on the inflamed gums.
- Tea Tree Oil: Tea tree oil has powerful antibacterial properties and can help reduce the bacteria that cause gum inflammation. Dilute a few drops in a glass of water and use it as a mouth rinse.
- Aloe Vera Gel: Aloe vera gel can be applied directly to inflamed gums and help relieve swelling and pain.
Mouthwash for gingivitis
Organic and natural antiseptic mouthwashes can promote a good bacterial balance in the saliva. We at Alpine BioDental do not recommend commercial mouthwashes, as they often contain harmful chemicals. We do recommend the use of mouthwashes which contain oxygen compounds. Similarly, oil pulling, a traditional Indian healing method used for centuries to improve overall oral health, is helpful in reducing harmful bacteria in the mouth, removing plaque and strengthening gums, which can help relieve gingivitis.
Professional teeth cleaning
Professional teeth cleaning helps to gently remove stubborn plaque and calculus that you cannot reach with normal cleaning equipment at home.
A subsequent full-mouth disinfection with ozone ensures a good microbiome in the oral cavity, as it promotes the growth of good, oxygen-loving (“aerobe”) bacteria and effectively eliminates the harmful, oxygen-hating (“anaerobe”) bacteria that like to colonise in the “pockets” (the area between the teeth and the gums) and cause gingivitis.
Myofunctional therapy
Often, chronic gingivitis can also be caused by mouth breathing, which evaporates the saliva. Without the protective immune cells in saliva, the oral mucosa is dried out and unprotected from bacterial attack. Using myofunctional therapy, nasal breathing can be trained on a neural level, which not only contributes to the health of your gums, but also reduces snoring, jaw joints and muscles (TMJ) disorders, muscle pain, and grinding and clenching.
Gum inflammation causes
The following are some examples of possible causes of gingivitis.
- Inadequate oral hygiene: If plaque and bacteria are not regularly and thoroughly removed from the teeth and gums, they can multiply and cause inflammation. We are happy to provide you with detailed advice.
- Poor oral flora: If there is a pathological oral flora, gingivitis is more likely to occur.
- Nutritional deficiencies: Inadequate intake of important nutrients, especially vitamin C and vitamin D, can make gums more susceptible to inflammation.
- Hormonal changes: Pregnancy, menstruation and menopause can lead to increased sensitivity of the gums and increase the risk of inflammation.
- Mouth breathing: Breathing through the mouth, especially at night while sleeping, can dry out the gums and lead to inflammation. Myofunctional therapy can make a big improvement in this area.
- Smoking: Smoking disrupts the normal function of cells and tissues in many ways. Nicotine for example constricts the blood vessels, therefore restricting the immune cells to enter and protect the gum tissue. As a result, gum tissue is more susceptible to infections such as gingivitis.
- Medications: Some medications, such as certain types of blood pressure medications, antidepressants, and anti-epilepsy medications, can increase the risk of gum inflammation.
- Stress: Chronic stress weakens the immune system and make the body more susceptible to infections, including gingivitis.
- Diabetes: People with diabetes are more susceptible to infections, including gingivitis, because high blood sugar levels can compromise the immune system.
- Autoimmune diseases: Autoimmune diseases such as lupus or rheumatoid arthritis can attack the gums and cause inflammation.
- Weak immune system: People with a weakened immune system, such as HIV or cancer patients, are more susceptible to gum inflammation.
Inflammation under crowns and implants
Bacterial plaque may adhere to insufficient crown margins, which you may find difficult to remove during oral hygiene. In this case, it is important to have the leaking crown replaced with a new, metal free, ceramic crown.
If you have different metals in the oral cavity (for example, amalgam fillings), an electric current can flow through the conductive medium of saliva. This also has a negative effect on the gums and promotes inflammation.
Inflammation of the gums and bone surrounding the implant, in medical terms called “peri-implantitis”, occurs frequently and should be controlled by an experienced dentist. Many precautions needs to be taken during the placement of dental implants to prevent peri-implantitis.
The symptoms of such an inflammation can be diverse. Common signs of inflammation under the crown includes pain, swelling, redness, or even an unpleasant taste in the mouth. However, in some cases, the inflammation may progress without any noticeable symptoms.
At the first signs of inflammation, home remedies can be a first aid to relieve symptoms. In the case of implant inflammation, for example, rinsing with a warm salt water solution or an antibacterial mouthwash can help to calm the inflammation and contain the spread of bacteria. However, always consult a (biological) dentist to determine the state of the inflammation and to treat this accordingly.
Difference between gum disease and periodontitis
When gingivitis is untreated, the inflammation progresses and attacks the connective tissues surrounding the teeth, called the “periodontium”. This inflammation of the periodontium is called “periodontitis”. Periodontitis is the advanced form of gum inflammation and this can have significantly serious consequences.
As the periodontium is the supporting structure between the tooth and its surrounding bone, inflammation of the periodontium leads to loss of bone support. This inevitably leads to tooth loss and other health complications. Unlike gingivitis, periodontitis is not completely reversible. However, it can be stopped and its progression can be prevented with professional dental treatment, improved oral hygiene and optimization of the bacterial flora in the mouth.
Gingivitis or periodontitis?
To determine the state of the inflammation and to diagnose whether it is gingivitis or periodontitis, we measure the “pocket” of the tooth. The point at which the gum normally separates from the tooth, creates what is called a “pocket.” In dental literature, a gum pocket greater than 3 millimetres is considered abnormal and potentially concerning.
The 3-millimeter limit comes from numerous studies and experiences of dental professionals. It is important to emphasize that gum pockets are normal and occur to varying degrees in many people. However, problems can occur when these pockets become too deep and it becomes difficult to clean them effectively, increasing the risk of gingivitis and ultimately periodontitis.
In general, pockets between 4-5mm are signs of gingivitis, and pockets of 6mm and higher are signs of periodontitis. It is important to note that even if a gum pocket is deeper than 3 millimetres, this does not necessarily mean periodontitis is present. However, it does indicate that additional care and possibly professional cleaning is needed to maintain and improve gum health.
Gingivitis during pregnancy
During pregnancy, hormonal changes in the body can cause gum inflammation, this is known as “pregnancy gingivitis”. Symptoms such as redness, swelling and bleeding of the gums can occur. Studies have shown that untreated gingivitis during pregnancy can increase the risk of premature birth or low birth weight. Therefore, it is important to maintain optimal oral health during pregnancy. Even before the onset of pregnancy, it is important to have a check-up to determine if there are any unnoticed pockets of inflammation in the mouth and if so, to have proper treatment.
Frequently asked Questions about Gingivitis
When it comes to the topic of gingivitis, there is a lot of confusion among patients. We have listed the common questions and answers for you.
It is recommended to have your restorations (crowns, fillings, inlays) checked for sufficiency by your dentist. It is also important to have the material they are made of checked. Careful oral hygiene is the key to prevent and treat gingivitis. This includes regular prophylaxis, ozone application to promote a good bacterial environment and regular check-ups and cleanings with the dentist.
Careful cleaning of the affected area in combination with disinfecting measures can provide quick relief. At home, you can also resort to natural painkillers. In any case, you should visit your dentist to diagnose and treat the causes.
If gingivitis remains despite good oral hygiene, it is important to see a dentist as soon as possible. Persistent inflammation can be a sign of more serious problems such as periodontitis.
Gum inflammation can occur anywhere in your mouth, but is often found in the area of the molars. This is because these areas are difficult to reach and are often overlooked during daily cleaning. They also often occur on insufficient restorations, metal restorations, or dead and root canal-treated teeth.
White gums can be a sign of gingivitis, but other conditions such as oral thrush can also cause this discoloration. Likewise, gums can take on a whitish color due to chemical burns, such as those caused by hydrogen peroxide.
If your gums are white and you have symptoms such as pain, swelling or bleeding, you should see a dentist.
In cases of chronic gingivitis, it is important to practice a good and consistent oral hygiene and have regular dental visits. Systemic causes should also be ruled out, such as autoimmune diseases or diseases of the gastrointestinal tract.
Dr. med. dent. Rebekka Hueber
Gum inflammation should be diagnosed and treated promptly. If you have any questions, please do not hesitate to contact us.

Further information
Further information intended to give a better overview of the topic.